Integrating Recruitment into eHealth Patient Records
Electronic health records are a viable alternative to today's subject recruitment methods.
Current practices for patient and investigator recruiting for clinical trials are inefficient and ineffective. This routinely results in scheduling delays, spiraling costs, and an increased risk of lower quality studies. These deficits are a serious problem for the drug research and approval process and ultimately hurt patients through delayed approvals and failure to identify safety risks. In addition, a declining number of physicians are willing to be investigators on clinical trials.
This article proposes integrating clinical trial recruiting with eHealth patient records by searching automatically for protocol qualified patients from among those who have consented to allow their records to be searched for such opportunities. This approach can be applied in today's environment, and then grow with the Regional Health Information Organization (RHIO) "movement."

The aggregation of eHealth records provides a way to identify patients, as well as potential investigators, for trials. Since this approach brings links to clinical trial information directly to the qualified patients and their physicians in the health care environment, it affords a "best practices" means of enrolling patients. Such eRecruiting and eHealth record integration will vastly improve the efficiency and selectivity of the recruitment process and can be extended to facilitate other aspects of clinical trial participation for investigators.
Lost opportunity costs
A retrospective benchmarking survey1 of 4000 clinical trials over a five-year period found that about half of the time spent on the trials was allocated to recruiting sites, investigators, and patients. Consistent with this, survey findings2,3 report that patient enrollments fall behind schedule in up to 86% of clinical trials, with 13% behind by more than six months. Moreover, delays in two or more stages of premarketing clinical trials have a compound effect and can result in cancellation of clinical research on potentially important medications.
As trial sponsors struggle to complete and maintain enrollments for premarketing clinical trials, the financial opportunity cost of inefficient and ineffective recruiting is the sales revenue that is not realized due to delays or outright failures in bringing new drugs to market. For example,3 for a new drug that is expected to generate a half billion dollars in annual sales, the sponsor will forgo sales of $1.3 million for every day the drug is not available for sale. Even when a trial fails to produce sufficient evidence of safety and efficacy, there is a financial opportunity cost if this conclusion is delayed by enrollment problems.
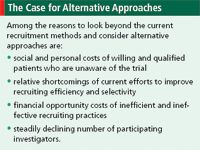
The Case for Alternative Approaches Case for Alternative Approaches
The social opportunity cost of inefficient and ineffective recruiting is the morbidity and mortality that could be avoided by new drugs coming to market sooner. In addition, too many patients are not aware of a trial for which they qualify. Just as sponsors have an incentive to minimize the operational costs of clinical trials, including recruiting, patients likewise have an interest in learning about trials that might improve their overall health and quality of life.
Investigator participation in trials
Studies4,5 have found that patient and physician investigator choices to participate in clinical trials depend on their expectations of the time and inconvenience that may be involved. A CenterWatch5 survey found that almost three-quarters of physicians interviewed had an interest in learning more about investigational treatments to supplement their knowledge. Yet, less than half of the physicians without clinical trial experience would refer patients to a clinical trial. For those who had clinical trial experience, 85% would refer their patients. The main reasons doctors gave for their lack of interest in trials were: a lack of information on clinical trials (58%), not enough time to learn about the trial (30%), and not knowing where to refer patients (28%).
The number of principal investigators in the United States fell 11.4% between 2001 and 2003, while the turnover rate nearly doubled. In a similar time frame, the number of domestic clinical trials declined by 10.6%,6 which conflicts with an increasing demand for clinical trials. The number of worldwide clinical trials for the year ending in March 2004 grew by 11.7%.7 The number of foreign investigators rose by 8%.6 Clearly, the United States has become a less desirable place to run trials, and the cost and resource incentives are to go "offshore" for investigators and clinical trials.8,9
Personalizing Notification Methods
Recruiting strategies
Within the United States, clinical trial sponsors are responding to the growing recruiting challenges with new strategies, including direct mail with call centers and Web sites, community outreach programs, and advertising. Advertising expenditures for trial enrollment in 2003 were $525 million. This is a $25 million (5%) increase over 2002, and the 2002 expenditure represented a 20% increase over the previous two years.10
There have also been substantial increases in the use of competitive enrollment practices, particularly financial incentives for sites that reach enrollment goals. A recent survey11 reports that 74% of sites employ competitive enrollment strategies. Of these, 78% receive bonuses for enrolling on schedule and 68% receive bonuses for overenrolling. Industry professionals, though, have criticized competitive recruitment practices, proposing that they create business interests that may conflict with good clinical trial practice.11
Another survey12 examined the productivity of alternative recruitment strategies. It found that the most successful method of notifying patients of an open enrollment was by mailings with a call center and Web site. This was followed by direct mail with a response card, patient database mailing, and specialty magazine advertising. Consistently, the highest number of responses is associated with the most efficient means of notification.
Patient responses to notifications of open enrollment do not mean that patients are willing to participate in the trial. Interestingly, none of the most efficient notification strategies was among the most productive for enrolling patients. The most productive strategies for enrolling patients were community outreach/health fairs and physician database mailings.
A comparison of the best strategies for eliciting responses and reliably enrolling patients strongly suggests that patients are most likely to participate in trials when the notification and supportive information are provided in a health care setting. The importance of involving the treating physician in the notification and explanation of available clinical trials is further illustrated in a study based on approximately 80,000 patient records from a heart disease clinical trial.13 This study compared physician referrals to screening patient records and then notifying protocol qualified patients directly. Identifying and notifying protocol qualified patients by screening coronary angiographic laboratory records had the highest volume, but less success at attracting patients to enroll. Physician referrals had the highest yield in attracting patients to enroll, but occurred at the lowest volume.
eHealth records in subject recruitment
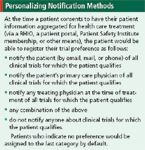
While most patients would want to know if they qualify for a particular trial, this cannot be generalized and is certainly not the case in all situations. To address this, based on discussions with patient and privacy advocates, we propose a patient-directed approach that maximizes opportunities to learn about trials, while retaining patient control over whether to be contacted about a clinical trial opportunity. Apart from the moral superiority of "opt-in" systems, patients who choose to be notified about trials for which they qualify are more likely to be comfortable and, presumably, more likely to enroll.
Patient-directed approach
Integrating clinical trial recruiting with eHealth patient records would involve the following:
- patients consenting to allow their eHealth records to be integrated with software that matches patient qualification and choice of notification (see sidebar) with the recruitment needs of a clinical trial
- notifying the patient and/or the patient's physician of available clinical trials that match with the patient
- providing the patient or physician with links to clinical trial sponsors for communication, support information, and procedures to enroll and participate.
No patient record information would be transmitted in the course of this recruitment process.
By integrating and scanning eHealth records and placing patients in control with the ability to change their minds or their notification choices, information about trials can be targeted to those who are both qualified and interested. Further, patients can have the information about appropriate trials go through the health professional they are most likely to turn to for advice on whether to enroll. Because of the "opt-in" feature, this approach to patient recruitment for clinical trials is protective of the patients' privacy and security. Additionally, the costs associated with this faster enrollment process can be covered by transaction fees paid by clinical trial sponsors who benefit from the greater efficiency and specificity of notification (via a trusted third party) to qualified patients with interest in learning about appropriate clinical trials.
Physician-enabled approach
Research on existing recruitment approaches (presented earlier) shows that an optimal recruiting strategy is based on notifying qualified patients of available clinical trials relevant to their health condition and ideally in consultation with a treating physician. The patient's decision to participate in a clinical trial is a health care decision. Treating physicians have access to the patient's records, have professional familiarity with clinical trials and treatment of the patient's condition, and, in most cases, have the trust of the patient. Treating physicians are generally the most qualified to consult with the patient about their medical situation and to inform them of the treatment options, including participation in a clinical trial.
The survey evidence reviewed shows that treating physicians are willing to refer patients to clinical trial enrollment if they have access to medical and logistical information. The combination becomes very powerful if this notification and decision process is handled in a patient-centric manner that preserves patient privacy and involves the treating physician. Streamlined processes, combined with eRecruitment strategies and information, offer the promise to retain current investigators and perhaps encourage new ones to participate in clinical research for the benefit of patients.
There are a number of considerations in setting up a trial with eHealth record recruitment. These include, but are not limited to, the following:
- Patient privacy: Patients must give consent to search their health records to determine eligibility for clinical trials (see also HIPAA requirements14 ).
- Data integration and aggregation: The more standardized the format of the data, the more opportunities for creating searchable databases. CDISC and HL7 have applicable standards and ongoing activities to support standard formats for protocol elements "tagged" as data. These groups are working together to harmonize standards for healthcare and clinical research, thus providing one portion of the infrastructure that will enable integration of eRecruitment with eHealth records.15
- Additional value for investigators beyond recruitment: Activities are in progress to enable the use of one computer system for health care and clinical research at an investigative site. The goal would be to eliminate the need for multiple systems—one per trial, each with a different log-in and different requirements for electronic data capture. Through the use of data standards and exchange formats, it is feasible to use the initial eligibility criteria and certain patient history and/or demographic data to prepopulate a case report form for the trial, thus reducing the transcription step (a potential source of error and added burden) for the physician or site personnel.
- Regulatory: The previous step described is a feasible methodology in today's regulatory environment. Entering additional trial data once to populate the eHealth record and the clinical trial database is also a process to streamline investigator involvement in the context of today's regulations (see the eSource Data Interchange (eSDI) document and the Single Source area of the CDISC Web site15 ).
- Technical aspects: Comparing eHealth records with potential trials is now a feature of some of the major electronic health record vendors and patient portals, as well as a planned feature by some of the developing RHIOs. The Patient Safety Institute is planning a demonstration of this capability in Knoxville, Tennessee. This indicates that the technical aspects are feasible in the current environment. Discussions are continuing to take place on how best to integrate the eHealth records with electronic data capture and data management for trials.
Conclusion
Integrating clinical trial recruitment with eHealth records has the potential for providing a very selective and reliable recruiting methodology, and substantially reducing the time required for recruitment. A study of a large cohort of controlled randomized clinical trials16 found that early success in recruiting is a reliable predictor of the likelihood of completing a clinical trial. "Best practices" recruiting through access to eHealth patient records will increase the speed and quality of enrollment and thus enhance the prospect for completing trials in a shorter time period. The widespread availability of recruiting based on eHealth patient record information could reduce recruiting times from years to weeks or days.
Clinical trial recruitment based on eHealth records will be especially advantageous in identifying protocol qualified patients with unusual health and medical characteristics. An additional benefit of eRecruitment is the potential to integrate it with the subsequent clinical trial data collection, which could facilitate investigator involvement and increase investigator participation in clinical trials.
ACTBITS
Carl Canavan, PhD, is a consultant from Arlington, VA, email: riskpref@mindspring.com Steven Grossman,* JD, is president, HPS Group, PO Box 10729, Silver Spring, MD 20914-0729, (301) 879-5600, fax (301) 576-5416, email: sgrossman@hpsgroup.com Rebecca Kush, PhD, is president, Clinical Data Interchange Standards Consortium, Austin, TX. Johnny Walker, MBA, is CEO of Patient Safety Institute, Plano, TX, www.ptsafety.org.
*To whom all correspondence should be addressed.
References
1. CMR International R&D Briefing: Benchmarking for Efficient Drug Development, 30 (2000).
2. J. Sullivan, "Subject Recruitment and Retention: Barriers to Success," Applied Clinical Trials,13 (April 2004).
3. N. Sinackevich and J.-P. Tassignon, "Speeding the Critical Path," Applied Clinical Trials, 13 (January 2004).
4. CenterWatch, "A 2003 Assessment of Competitive Trial Enrollment Practices," Pharmaceutical R&D Statistical Sourcebook 2004/2005, p. 109.
5. CenterWatch, "Physician Referrals Into Clinical Trials: A 2004 Assessment," Pharmaceutical R&D Sourcebook 20004/2005, p. 111.
6. K. Getz, "Number of Active Investigators in FDA-Regulated Clinical Trials Drop," Tufts Center for the Study of Drug Development, CSDD Impact Report (May/June 2005).
7. K. Getz, "Are We Pushing Our PIs Too Far?" Applied Clinical Trials, 14 (September 2005).
8. "Clinical Studies Employing Both U.S. and Non-U.S. Sites Rise—FDA Study," Pharmaceutical R&D Statistical Sourcebook 2004/2005, p. 110.
9. Office of Inspector General, "The Globalization of Clinical Trials: A Growing Challenge in Protecting Human Subjects," Department of Health and Human Services, September 2001.
10. "The Reasons People Participate in Clinical Trials," Pharmaceutical R&D Sourcebook 2004/2005, p. 112.
11. CenterWatch, "A 2003 Assessment of Competitive Trial Enrollment Practices," Pharmaceutical R&D Statistical Sourcebook 2004/2005, p. 109.
12. B. Harper, "Understanding the Effectiveness of Patient Recruitment Programs: What Have We Learned?" Pharmaceutical R&D Statistical Sourcebook 2004/2005, p. 109.
13. E. Handberg-Thurmond, A. Baker, M. Coglianese et al., "Identifying High Yield Sources of Patients with Coronary Artery Disease for Clinical Trials: Lessons from the Asymptomatic Cardiac Ischemia Pilot (ACIP) Experience," Clinical Cardiology, 21 (3), 177–182 (1998).
14. http://www.cms.hhs.gov/hipaa/.
15. www.cdisc.org; www.hl7.org; www.bridgproject.org.
16. A.-B. Haidich and J. Ionnidis, "Patterns of Patient Enrollment in Randomized Controlled Trials," Journal of Clinical Epidemiology, 54, 877–883.

Patient and Site Personnel Perceptions of Retail Pharmacy Involvement in Clinical Research
March 7th 2024Despite industry-wide excitement over the involvement of retail pharmacies in clinical research, there is little information currently available on how retail pharmacies are perceived by investigative sites and patients.