Comparison of Androgen Receptor Inhibitors for Nonmetastatic Castration-Resistant Prostate Cancer Shows Advantage with Darolutamide
Cohort study finds a superior tolerability profile with darolutamide compared to other androgen receptor inhibitors, which investigators said indicates an efficacy advantage in the treatment of nonmetastatic castration-resistant prostate cancer.
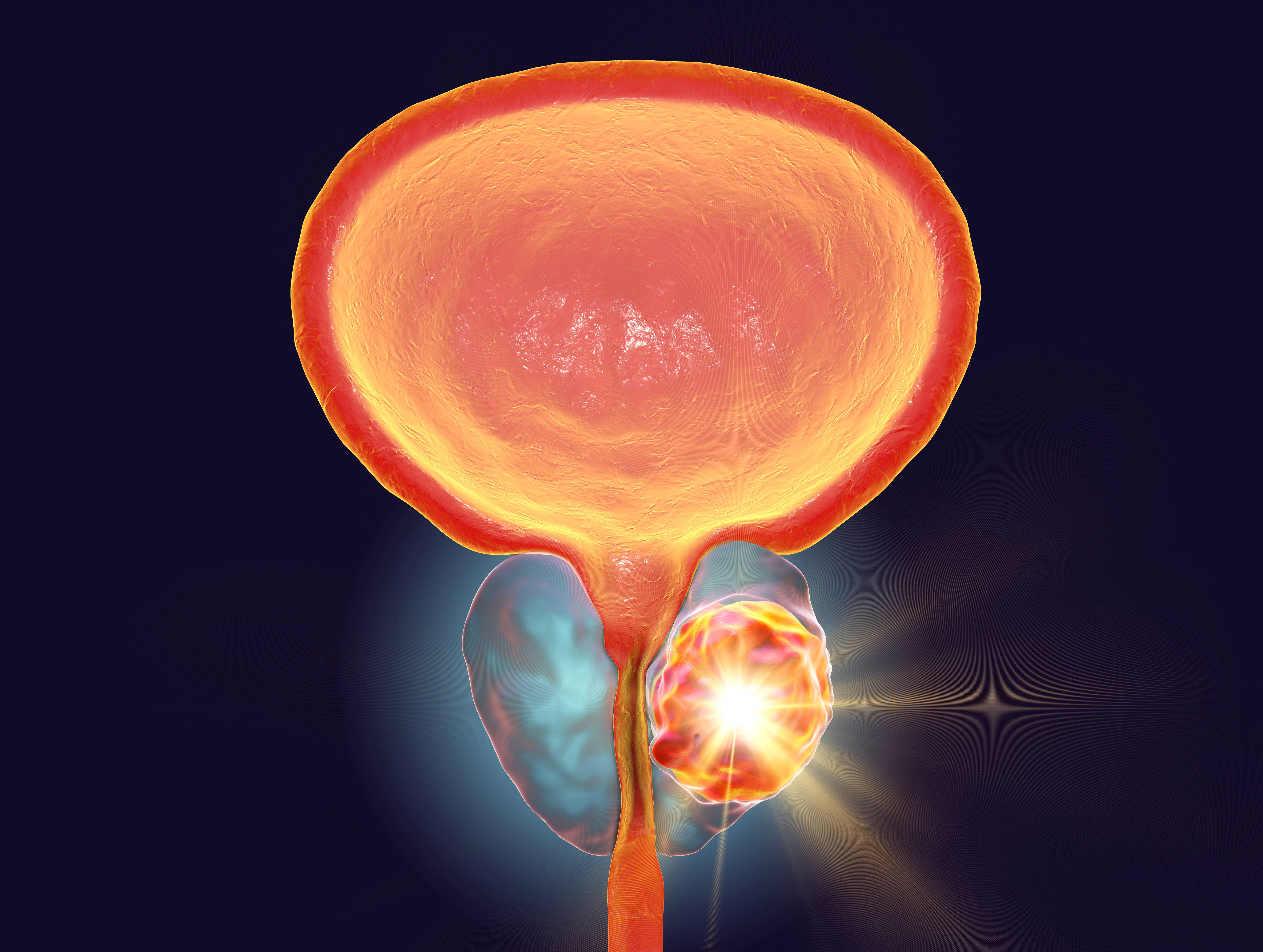
Image credit: Dr_Microbe | stock.adobe.com
A cohort study comparing outcomes with the use of darolutamide (Nubeqa), enzalutamide (Xtandi), and apalutamide (Erleada) in the treatment of nonmetastatic castration-resistant prostate cancer (nmCRPC) showed superior tolerability with darolutamide. According to the authors of the study, published by The Journal of the American Medical Association, the findings may be indicative of a clinical efficacy advantage for darolutamide over the other analyzed androgen receptor inhibitors (ARIs) in the treatment of nmCRPC.1
“For patients who develop (nmCRPC), 3 novel androgen receptor inhibitors (ARIs; darolutamide, enzalutamide, and apalutamide) are approved standard-of-care treatment options based on randomized, double-blinded, placebo-controlled clinical trials demonstrating improved metastasis-free and overall survival,” the study authors wrote. “However, nmCRPC usually develops in older men with significant prior exposure to androgen deprivation therapy, potentially increasing patient frailty beyond physiologic age. Consequently, treatment discontinuations among patients receiving ARIs are common due to adverse events (AEs), with discontinuation rates due to AEs in pivotal phase 3 trials ranging from 9% to 17% in treatment groups compared with 7% to 9% in placebo groups.”1
Of the analyzed drugs, enzalutamide had the most recent regulatory action, having been approved by the FDA to treat nonmetastatic castration-sensitive prostate cancer with biochemical recurrence at high risk for metastasis.2 The approval was based on findings from the Phase III EMBARK trial (NCT02319837), which demonstrated that the addition of enzalutamide to leuprolide reduced the risk of metastasis or death by 58% compared to leuprolide monotherapy.3
“Since regulatory approvals of ARIs in 2019, scant data are available to describe the use and tolerability profiles of the 3 ARIs in clinical practice,” the authors of the current study wrote. “In the absence of head-to-head randomized clinical trials, comparative clinical experience can inform expectations and treatment choice for clinicians managing a broad spectrum of patients, who may differ from clinical trial participants.”1
To conduct the analysis, the investigators evaluated electronic medical records from the Precision Point Specialty network of urology practices in the United States. Three cohorts were included and were defined by first ARI use from among darolutamide, enzalutamide, or apalutamide to treat nmCRPC.
Patients were 18 years of age or older at the index date with treatment initiated with darolutamide, enzalutamide, or apalutamide between August 1, 2019, and March 31, 2022. The primary outcome of the study was a composite of two endpoints—treatment discontinuation and progression to metastatic CRPC (mCRPC), whichever occurred first.
A total of 870 patients met the eligibility criteria, with 362 patients administered darolutamide (41.6%), 382 administered enzalutamide (43.9%); and 126 administered apalutamide (14.5%).
The darolutamide cohort showed lower proportions of patients with a composite endpoint event (134 [37.0%] vs 201 [52.6%] for enzalutamide and 66 [52.4%] for apalutamide). In terms of discontinuation, there were 110 (30.4%) patients in the darolutamide cohort who discontinued treatment, compared to 156 patients (40.8%) in the enzalutamide cohort and 58 patients (46.0%) in the apalutamide cohort. Progression to mCRPC was observed in 64 patients (17.7%) in the darolutamide cohort, compared to 108 patients (28.3%) in the enzalutamide cohort, and 35 patients in the (27.8%) apalutamide cohort.
After adjusting for baseline covariates, investigators found that patients in the darolutamide cohort were also found to have a lesser risk of a composite endpoint event compared with the enzalutamide cohort (risk reduction, 33.8%; hazard ratio [HR], 0.66 [95% CI, 0.53-0.84]) and the apalutamide cohort (risk reduction, 35.1%; HR, 0.65 [95% CI, 0.48-0.88]). Further, the darolutamide cohort showed a lower risk of discontinuation compared to the enzalutamide cohort (risk reduction, 27.4%; HR, 0.73 [95% CI, 0.56-0.94]) and the apalutamide cohort (risk reduction, 39.1%; HR, 0.61 [95% CI, 0.44-0.85]).
There was also a lesser risk of progression to mCRPC in the darolutamide cohort compared to the enzalutamide cohort (risk reduction, 40.6%; HR, 0.59 [95% CI, 0.43-0.82]) and the apalutamide cohort (risk reduction, 35.3%; HR, 0.65 [95% CI, 0.42-0.99]). No differences were observed between the enzalutamide and apalutamide cohorts across outcomes.
“Although a causal link cannot be established between the better tolerability profile of darolutamide and its clinical effectiveness advantage compared with enzalutamide and apalutamide, this association was observed across multiple outcomes and appears consistent,” the study authors wrote. “Because the 3 ARIs demonstrated similar efficacy in their respective phase 3 trials, extended treatment durations in clinical practice may confer a benefit in delaying mCRPC progression.”1
References
1. George DJ, Morgans AK, Constantinovici N, et al. Androgen Receptor Inhibitors in Patients With Nonmetastatic Castration-Resistant Prostate Cancer. JAMA Netw Open. 2024;7(8):e2429783. doi:10.1001/jamanetworkopen.2024.29783.
2. Pfizer and Astellas' XTANDI® Approved by U.S. FDA in Earlier Prostate Cancer Treatment Setting. Astellas Pharma Inc. News release. November 17, 2023. Accessed August 28, 2024. https://www.astellas.com/en/news/28626
3. Freedland SJ, de Almeida Luz M, De Giorgi U, et al. Improved outcomes with enzalutamide in biochemically recurrent prostate cancer. N Engl J Med. 2023;389(16):1453-1465. doi:10.1056/NEJMoa2303974. Accessed August 28, 2024.
Newsletter
Stay current in clinical research with Applied Clinical Trials, providing expert insights, regulatory updates, and practical strategies for successful clinical trial design and execution.
Unifying Industry to Better Understand GCP Guidance
May 7th 2025In this episode of the Applied Clinical Trials Podcast, David Nickerson, head of clinical quality management at EMD Serono; and Arlene Lee, director of product management, data quality & risk management solutions at Medidata, discuss the newest ICH E6(R3) GCP guidelines as well as how TransCelerate and ACRO have partnered to help stakeholders better acclimate to these guidelines.
Managing Side Effects and Dosing in Off-Label GLP-1 Use with Help from Real-World Evidence
July 18th 2025Shipra Patel, global therapeutic area section head, endocrinology, global head, pediatrics, Parexel, explains how real-world data is helping researchers navigate gastrointestinal side effects, dose flexibility, and long-term tolerability in off-label GLP-1 use.
Anselamimab Misses Primary Endpoint in Phase III CARES Trials for AL Amyloidosis
July 17th 2025In the Phase III CARES trials, anselamimab did not meet the primary endpoint for advanced-stage AL amyloidosis, but a prespecified subgroup analysis revealed meaningful improvements in survival and cardiovascular outcomes.