Overcoming the Paradox of Choice: Selecting EDC Capabilities to Fit Your Needs
Brand Insights - Thought Leadership from Marketers I Paid Program
Welcome back to the Forum for EmergingBio's Outsourcing Decisions!
In our last blog, we discussed how to avoid and reduce the impact of momentum-breaking clinical trial amendments. One of the key ways to mitigate this risk is choosing the right electronic data capture (EDC) system to collect and manage your clinical trial data. The challenging part about this seemingly simple task is that it can quickly become very overwhelming. Sponsors will often express frustration, saying things along the lines of “the process started out well, but, now that I have spoken to a few service providers, everything is starting to blur.” With so many EDC providers offering a range of solutions, how can startups or small biotechs ensure they select the right tools with the capabilities to fit both existing and future needs? How do you begin to sort through all the choices and find the right EDC platform or solution?
As with any investment, you need to do some homework before making a decision. I sat down with Richard Young, Vice President, Vault CDMS Strategy at Veeva Systems, to discuss what that entails when it comes to shopping around for an EDC and how sponsors within smaller organizations can ensure they are set up for long-term success.
Below are some questions that often come up in our conversations with clients about the EDC-selection process and our thoughts on how sponsors can best address them.
What questions should sponsors ask as they evaluate EDC solutions?
Tanya: It’s important to begin by asking what functionality is necessary. This may seem obvious, but this critical step often gets missed. It’s very easy to be lured in by the bells and whistles many systems offer, but do they address your company’s needs for specific studies? Identify these needs and then analyze and prioritize them. Doing so will help you narrow down and simplify the criteria on which to base your decision and how to potentially adjust your budget. The next subject to tackle is whether the EDC integrates with other systems in your technology portfolio and how the EDC vendor’s pricing fits in with your budget.
Richard: Absolutely. Once you have this information in hand and set key priorities, there are several other questions that should also be kept top of mind. For example: Is the system easy to use? Does the system fully support compliance with CFR Part 11? How long will it take to implement the system? What kind of training and support services does the vendor offer?
A solution that is easy to use, with an intuitive design, will simplify complexity. During demos, be sure to inquire about a straightforward way to set up a protocol, accurately enter data and efficiently manage queries. It’s also critical to get ahead of potential compliance issues by making sure the system fully supports CFR Part 11.
What about a service provider or vendor’s experience? Is that a critical factor?
Tanya: Experience is always an important factor. We encourage our clients to take vendor stability into consideration. What you want to know is that the service provider is going to be there for you in the long run by investing in its technology, adding and enhancing capabilities to support innovation, scaling needs and long-term growth.
Richard: Asking about a vendor’s experience is essential. But it is equally important to recognize that, within the world of clinical trials, our current processes are broken and require new thinking and new technologies. As an industry, we have become experts in creating workarounds and patches using traditional EDCs that mimic paper. What’s happened is that these limited, old-fashioned tools now dominate our data collection strategies, creating distractions that waste time and money. A broad range of service providers and suppliers offer EDC, as it has become the “industry standard,” however the features and functions that separate “traditional” and “modern” EDCs are worlds apart. It’s important to find a technology partner that can offer fully integrated APIs for other systems, flexible and automated workflows, and productized functionality as opposed to external custom functionality. A modern EDC creates a unique, bespoke and tailored user experience for each stakeholder involved in clinical trial data collection and management.
In addition to experience, what are the top considerations an emerging company must consider when selecting a technology partner?
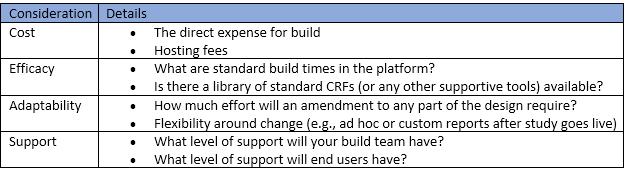
Tanya: It comes down to cost, efficacy, adaptability and level of “after-sale” support available. We encourage our clients to carefully consider the following:
Richard: Great question. First, you need a technology that enables you to run the trial you wish to perform, not the trial that the technology will limit you to. The high cost of making changes in traditional EDCs has anchored our vision to one-dimensional studies for too long. Modern trials are multi-dimensional and fluid in execution.
Second, you need a partner who will genuinely invest in your success. Collaboration is the key to delivering trials successfully and that starts with true partners coming together, working together and, of course, problem solving together. For me, this starts with technology that provides greater agility and extends through a delivery team that is caring and responsive to the sponsor’s needs. Every vendor should be attentive during the sales cycle and read through recent customer case studies to get a better sense of customer needs.
What are the main causes of database-build delays? And how do sponsor and CRO cycle times compare for database build, data entry and database lock?
Tanya:There are several factors that contribute to database delays, but typically we see three main causes: (1) building on unclear protocol specifications, (2) building on unclear database design specifications (if applicable); and (3) technical restraints within an EDC platform that require a lot of customizations (and thus additional manual programming or work-around solutions). The first two causes result in numerous back-and-forth discussions around designs of forms, edit checks and many drafts of the CRF/edit checks. While the third cause is more technical, it requires manual effort (and continuous problem solving), which can be a real source of frustration when everything else is in place to expedite a study build.
Richard: This is a tricky question, as it really depends on when you start and stop the clock. From my perspective, the clock starts when you have a “good” draft protocol, which can be used in a meeting kicking off an engagement between sponsors and their service provider partners. For a traditional EDC study build, it typically takes sponsors 12-18 weeks and CROs 8-12 weeks. Both timelines are far too long.
According to research conducted by the Tufts Center of Drug Development in 2017-2019, protocol changes are the primary cause of delay during database builds. The impact of these changes is amplified by other common causes, which are User Acceptance Testing (UAT) and limited design functionality. Securing consensus among stakeholders is difficult and time consuming. Therefore, it is critical to select an EDC with design tools that support collaborative decision making and real-time changes.
There are numerous differences that account for different cycle times among sponsors and CROs, but the most common factors that extend database lock times have to do with the growing volume of data coming from external sources.
What are the best ways to overcome clinical data management challenges including protocol changes, reporting and more?
Tanya: Ensuring you have libraries and standards to work from at study startup is a huge help, even if these need to be customized for specific protocols because they save considerable time. Of course, amendments are often unavoidable and therefore managing them must be considered when selecting an EDC. When it comes to amendments, some platforms are much more nimble than others.
Richard: Put simply, select a flexible solution that embraces the need for change. Look for purpose-built capabilities to manage change, such as casebook versioning so investigator sites can adopt the latest version as soon as they receive IRB approval. Another example would be push-button deployments, such that any and all changes can be deployed in minutes, without migrations or downtime for sites.
Agile trial design is an important factor when planning clinical studies. How can companies address and build this into their data management processes successfully?
Tanya: First and foremost, by selecting an EDC platform that allows for more agile trial design. Once that’s in place, sponsors must ensure that the teams working on the trial understand how agile design can be utilized to bring efficiency to the entire study process. This means understanding the end user’s experience as well as the data management cleaning, and quality-by-design concept that is required by regulatory authorities.
Richard: An agile build process fosters better collaboration and decision-making within the study team. Rapid iterations help you achieve user acceptance up-front, early in the build, which reduces late-stage changes as well as findings during UAT. Your technology should provide reports with efficiency and effectiveness metrics. These then inform decisions on what works and what doesn’t, so you can course correct and move forward decisively.
Do you have any final advice for those going through the vendor selection process?
Richard: Ask questions, a lot of questions. Ask to see and experience the features you need, and then ask the technology company (and their CRO partner) what else they can show you. Beyond that, dare to think fresh, dare to park the old methods and seek a better way. Technology is moving fast, faster than you may even imagine. Good technology can support your trial design and execution goals in ways that you may not yet have considered. We used to design trials and then ask how we can deliver them, but today, we can ask what technologies can do for us, and then look at how we can use these features to better our research.
Tanya: Approach your vendor selection process with structure and purpose. Make sure you know what you need from the system, what you would like and what would be the absolute best-case scenario to meet your needs, for all stakeholders—data mangers, clinical teams and, of course, the research sites. With this knowledge in hand, you can be more specific with service providers about what capabilities to show you during demos and avoid generic presentations. Following this approach will make it easier for you to do an apples-to-apples comparison and assess which EDC service provider offers the best fit and is the right choice for you.
In our next blog, we’ll talk about how to leverage standards to increase clinical trial efficiency and reduce costs. Companies may think they are too small to establish standards, or are feel overwhelmed by the thought of setting them up. However, there are easy ways to build standards into the process without incurring significant costs. Stay tuned for more on that!
Tanya du Plessis is vice president of data strategies and solutions at Bioforum the Data Masters. She has vast experience across the industry through her current role at Bioforum, as well as the 14 years she spent with IQVIA (legacy Quintiles). Throughout her career, Tanya has worked with multinational pharmaceutical companies as well as small-to-mid size biotechs and startups. She has led various data management operations and programs, heading numerous innovation teams and spearheading the development of strategies for customized data delivery solutions, focusing on timely, quality data. tanya.duplessis@bioforumgroup.com
A certified clinical data manager (CCDM, SCDM), Tanya holds a M.Med.Sc in Hematology and Cell Biology from the University of the Free State in South Africa. She also has a project management professional certification (PMP, PMI).
About Bioforum the Data Masters
Bioforum the Data Masters is a data-focused Contract Research Organization (CRO), supporting clients in the utilization of their clinical data and guaranteeing its integrity and accuracy. Our goal is to consistently improve and innovate data processes to allow for the most efficient data submissions for our clients across the life sciences industry and the patients they serve.
How Small Biotechs Can Overcome Study Execution Challenges and Achieve Big Results
Regret Comes Too Late: Getting Ahead of Protocol Amendments
September 8th 2020Welcome back to the Forum for EmergingBio's Outsourcing Decisions! There is nothing quite like protocol amendments to put the brakes on a clinical trial’s momentum, which is why, in this blog, we are turning our attention to how to face this challenge head on.
Bioforum, the Forum for EmergingBio's Outsourcing Decisions
June 30th 2020As the biopharma industry traverses unchartered waters amid the COVID-19 crisis and doubles down on its efforts to bring new therapies to market faster, cheaper and without affecting quality, the success of strategic partnerships and functional service provider models will become more critical than ever before.